More than half of women having babies will be given epidurals to block pain during labor. Despite the general acceptance and proven safety of today's epidurals, however, many women still agonize over whether to accept one. For most expectant moms, the turmoil is due to two issues: They might feel as though they're being "weak" if they opt for anesthesia when they give birth, and secondly (and more importantly), they fear for their own safety and for the safety of their babies.
This blog was excerpted from an article titled "Epidurals: 6 Things You Need to Know." This article was published on fitpregnancy.com and can be found here.
Epidurals work to block pain like this: Nerves carrying pain signals all have to travel through the "epidural space" on their way to your brain. Imagine each nerve traveling through a sort of two-layer sleeve; the space between the layers is the epidural space. Therefore, anesthesia can be injected into this area to block those pain signals, and voila! You're pain-free.
Everyone experiences pain differently; the intensity of the pain has nothing to do with who is tougher. If you're considering an epidural, here are answers to the most common questions about the procedure—starting with how an epidural can affect you and your baby.
1. What effect will an epidural have on my baby and me?
Although epidurals don't slow down dilation of the cervix or increase your risk of needing a Cesarean section, they might prolong the pushing phase of delivery by an average of 20 minutes. The procedure also can increase your temperature and increase your chances of developing a fever. This can confuse your doctor, who might not be able to tell whether the increase in temperature is because of the epidural and not cause for concern or due to an underlying infection that could be transferred to your baby.
The upside of an epidural is related to the body's normal reaction to pain. Pain causes the release of stress hormones into the bloodstream, which can increase your heart rate and divert blood from the uterus. Pain can also make you hyperventilate, which can also divert blood away from the placenta, the part of the uterus where your baby gets oxygen and nutrients. As epidurals block this pain from happening, you don't suffer its ill effects.
As for the health of your baby, researchers haven't found a significant difference in APGAR scores or the results of other specialized tests of babies born to mothers with labor epidurals and babies born to mothers who did not receive any medications during labor.
2. Will it hurt?
Although some women fear getting epidurals more than they fear childbirth, after getting one, most say that the procedure is less uncomfortable than an IV or even one contraction. Many understandably worry about the size of the needle, but the size of the epidural needle ultimately doesn't matter. This is because an initial, truly tiny needle is used to numb the area just before the epidural needle is inserted. Most women don't mind this tiny needle. They do, however, feel the numbing medication that is injected through the needle. This will sting for about five seconds. The epidural medication starts to work within five minutes and peaks in 10 minutes. Therefore, it will typically take about 15 minutes from the moment we start the procedure to the moment you feel relief from pain.
3. How is an epidural performed?
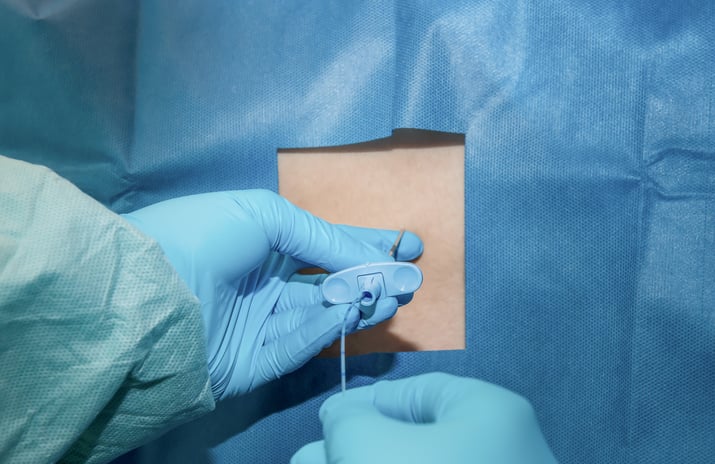
We position some women on their sides and ask other women to sit up during an epidural. You probably won't be offered a choice. Either way, your OB nurse will help get you into the necessary position. Cleaning solution is swirled on your skin, the numbing medication is injected and the epidural needle goes through the numb area (and you feel a little bit of pressure). The epidural catheter is threaded into your epidural space (with either no pain or possibly a one-second "hit- your-funny-bone"–like sensation down a leg), the needle is removed, and the catheter is taped to your back. You lie down (but you can't feel the thin catheter), meds are pushed through the catheter, and, finally, you're connected to a pump that continually replenishes the epidural medication until you deliver.
4. What happens if I move or have a contraction during an epidural?
Labor contractions can be as frequent as every two minutes; it's unlikely that an epidural could be put in place between contractions that are coming this fast. You'll have a couple of contractions during placement, but it's OK—placing an epidural is not an extremely delicate process. Women who make a small to moderate movement during the procedure slow us down, but almost everyone can stay still enough.
 via shutterstock.com |
5. How do you know you're in the right place and not hitting my nerves or spinal cord?
We know we're in the epidural space because we feel a change in the syringe attached to the epidural needle. When your anesthesiologist finds your epidural space—and finding it can take as little as 60 seconds—he or she will thread the epidural catheter in.
A common misconception is that the epidural (or spinal) is placed into a nerve or into the spinal cord. Nothing could be further from the truth. The needle, catheter and medication go into the compartment that the nerves pass through.
Your spine is a protective bone structure surrounding your epidural space. Bumping into the spine (the bone) with the epidural needle should not hurt. In fact, you probably wouldn't realize it if your anesthesiologist bumps into the spine. Also, know that it's extremely difficult to bump any nerves, especially your spinal cord, with the epidural needle. The nerves enter the epidural space from the sides, not from the center—and the needle is placed in the center.
6. Will I be able to walk around after the epidural?
Your legs may feel tingly and a little weak by this time, so it's not safe for you to be moseying through the halls. (Some hospitals offer "walking" epidurals, which initially don't limit you to your bed as much.) For most, plan on staying bed-bound for the rest of your labor. Besides, your obstetric team will want to monitor your baby's heartbeat frequently, which needs to be done from bed.
This blog was excerpted from an article titled "Epidurals: 6 Things You Need to Know." This article was published on fitpregnancy.com and can be found here.



